Developing my research question
The first step in a research project is to develop the question you seek to answer. I thought I developed my research question many months ago. In the halls of Frost Library at Amherst College; through conversations with my advisors as I worked on my undergraduate thesis on health care delivery models in South Africa; in my New York City apartment as I refined my Fulbright Statement of Grant Purpose. I don’t want to dismiss these activities, for they will certainly have contributed immensely to the development of my research question, objectives, methods and so on. However, it was through two back-to-back visits to Vulindlela, a sub-district 150 km north-west of Durban, that I feel I have truly begun the process of uncovering my research question.
Vulindlela is a largely Zulu-speaking rural community that is home to about 90,000 residents. The HIV prevalence rate in this rural community is astoundingly high. Just under a third of women ages 25-29 are infected with HIV, and this increases to 46.8% for the cohort of women ages 30-34 (Karim et al., 2011). Among certain age cohorts, women in Vulindlela are more likely to be infected with HIV than her counterparts in Durban (an urban city). For example, a woman between the age of 30 and 34 who lives in Vulindlela is 1.4 times as likely to be infected with HIV compared to a similarly aged woman living in Durban. Her biggest risk factors: she is poor, uneducated and unable to negotiate safe sex with her partner. See the table below for a more comprehensive set of data from the study.
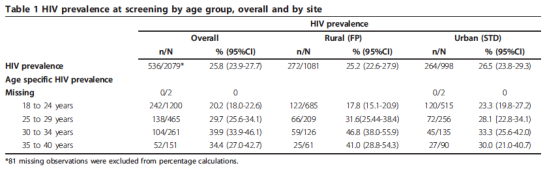 (Snapshot of Table 1 from Karim et al., 2011)
(Snapshot of Table 1 from Karim et al., 2011)
Vulindlela has seven Primary Health Care (PHC) clinics where nurses provide comprehensive primary care, including family planning services, voluntary HIV counseling and testing, STI treatment, antenatal care and a whole host of other services. Caprisa has been working in Vulindlela for 10 years, providing HIV prevention, treatment and care to the community at its clinical research site.
Making your research relevant
As a result of the PEPFAR transition, all NGO’s providing PEPFAR-funded care and treatment have recently been required to down-refer their patients to department of health PHC clinics. This additional patient load will likely impose a significant burden on already overstretched and under-resourced clinics. These issues are particularly pertinent when it comes to patients on antiretroviral therapy (ART), whose health depends upon adherence to their drugs and clinical management of side effects. As Caprisa transitions its patient load to the seven PHC clinics in Vulindlela, several research questions come to mind:
- What are the human resource for health figures of the seven Vulindlela PHC clinics?
- How many NIM-ART nurses are there, and how are they balanced among the PHC clinics?
- How does the level of support to NIM-ART nurses from clinicians vary by urban versus rural facilities? Does this impact health outcomes?
Vulindlela is one community among hundreds in South Africa that is facing the dual burden of imbalances of human resources for health and high rates of HIV. While private NGOs such as Caprisa have filled a critical gap for many years, the department of health is primed to step up its responsibility for health care provision. It is the confluence of these factors and events that will help shape my research questions in the coming weeks. Stay tuned!
